Higher Prevalence of Autism Among Siblings: A BCBA’s Insights on New Research Findings
I often find myself diving into the latest research to better understand the complexities of autism spectrum disorder (ASD) and how it affects our clients and their families. Recently, I came across a compelling study by UC Davis MIND Institute researcher Sally Ozonoff and the Baby Siblings Research Consortium that sheds light on the likelihood of autism in siblings of autistic children. The study found that siblings of autistic children have a 20% chance of being autistic themselves, which is about seven times higher than the rate in infants with no autistic siblings.
This significant finding is backed by a large, diverse group of families from research sites across the United States, Canada, and the United Kingdom. The study confirms previous research from 2011 by the same group, which found a recurrence rate of 18.7%, now slightly increased to 20.2%.
One of the most striking aspects of this research is the influence of the sex of the first autistic child on the likelihood of recurrence. If the first autistic child is a girl, the family is 50% more likely to have another child with autism compared to families where the first autistic child is a boy. This suggests genetic differences that could increase recurrence likelihood in families with an autistic daughter.
Moreover, the study found that a child with multiple autistic siblings has a higher chance of being diagnosed with autism (37%) than a child with only one autistic sibling (21%). This is particularly relevant for us as we consider the genetic and environmental factors that might influence autism recurrence in our client families.
The sex of the infant also plays a role. Boys born after an autistic sibling are almost twice as likely to be diagnosed with autism compared to girls. This aligns with the general observation that boys are diagnosed with autism about four times more often than girls. In practical terms, this means we need to be especially vigilant in monitoring the development of younger siblings, particularly boys, in families already affected by autism.
Another layer of complexity is added by factors such as race and maternal education level. The study found that non-white families have a higher recurrence rate (25%) compared to white families (18%). Additionally, families where the mother has a high school education or less see a recurrence rate of 32%, which decreases with higher levels of maternal education.
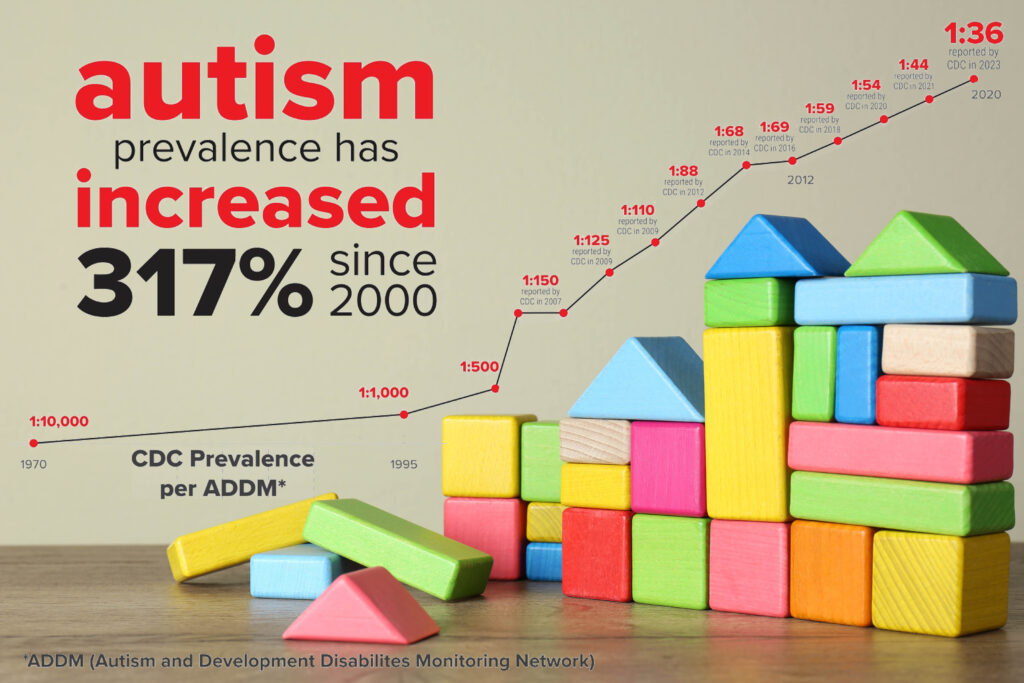
These findings are new and critical to replicate, but they mirror recent CDC data indicating that autism is becoming more prevalent in historically underrepresented groups. This reversal of a longstanding trend highlights the potential social determinants of health that could lead to higher rates of autism in certain families.
The researchers also tracked families who dropped out of the study, finding no significant difference in outcomes compared to those who completed it. This reassures us that the estimates of recurrence are reliable.
For us at the clinic, these findings reinforce the importance of closely monitoring the development of siblings of autistic children, especially in families with reduced access to care. Early diagnosis and intervention are crucial for improving outcomes. This study serves as a reminder of the importance of our work and the need to stay informed about the latest research to provide the best support for our clients and their families.